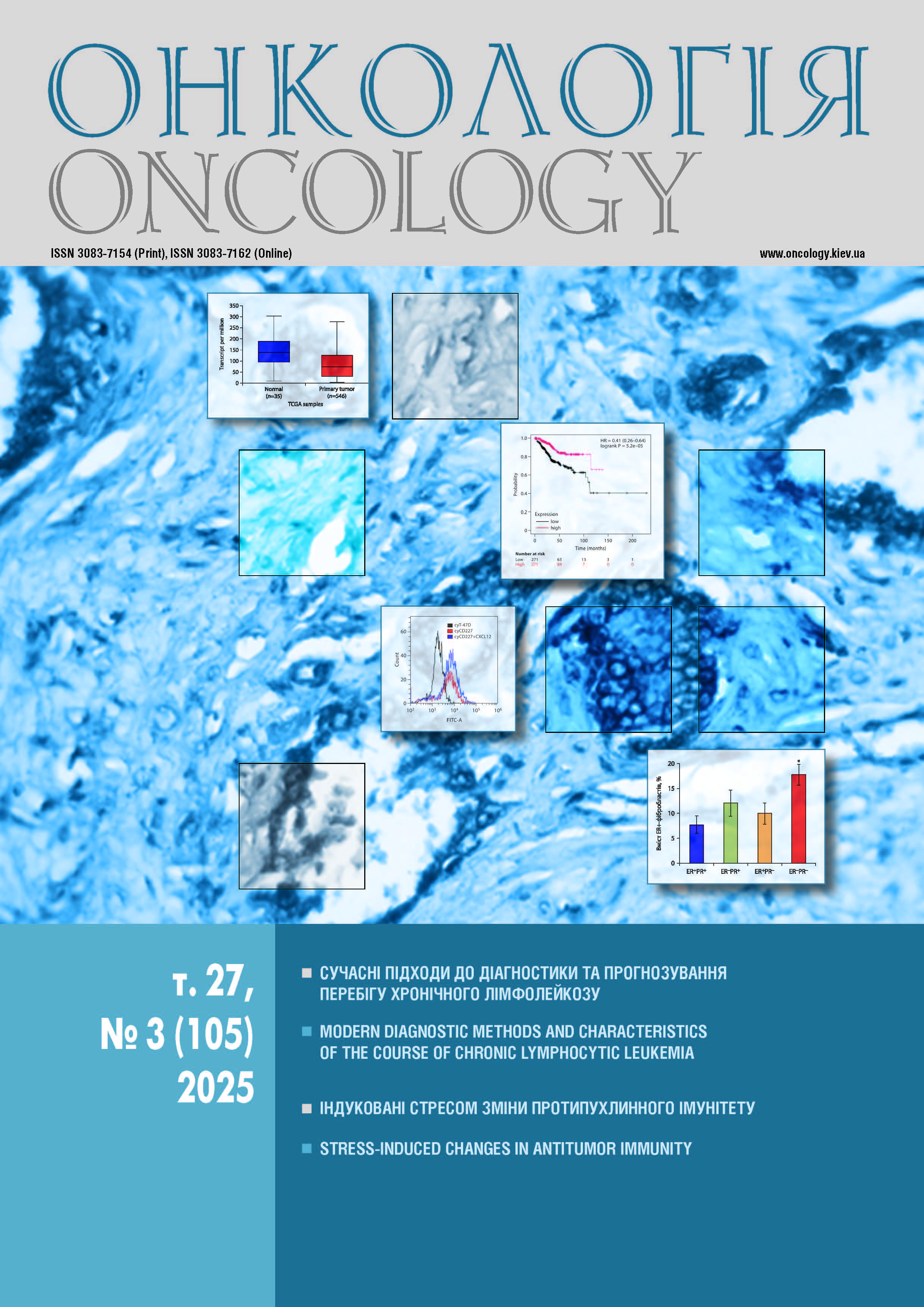
СТРЕС-ІНДУКОВАНІ ЗМІНИ ПРОТИПУХЛИННОГО ІМУНІТЕТУ
DOI:
https://doi.org/10.15407/oncology.2025.03.161Ключові слова:
стрес, рак, катехоламіни, глюкокортикоїди, мікроелементи, протипухлинний імунітетАнотація
Результати експериментальних та клінічних досліджень свідчать про значний модифікуючий вплив стресу на функціонування як окремих фізіологічних систем, так і організму в цілому, що не тільки підвищує ризик виникнення злоякісних новоутворень, а й може негативно впливати на результати лікування пацієнтів з цією патологією. В оглядовій статті авторами представлено аналіз даних сучасної наукової літератури щодо взаємозв'язку між стресом і онкогенезом, представлені стрес-індуковані зміни вмісту основних мікроелементів (мідь, залізо, цинк, ферум, кальцій), які відіграють ключову роль у багатьох біологічних процесах. Значна увага приділяється змінам функцій імунокомпетентних клітин, що входять до складу пухлинного мікрооточення та опосередковують реалізацію протипухлинної імунної відповіді, в умовах гострого та хронічного стресу.
Посилання
Orive M, Barrio I, Lázaro S, et al. Five-year follow-up mor- tality prognostic index for colorectal patients. Int J Colo- rectal Dis 2023; 38: 64. https://doi.org/10.1007/s00384- 023-04358-0.
Yang T, Qiao Y, Xiang S, et al. Work stress and the risk of cancer: A meta-analysis of observational studies. Int J Can- cer 2019; 144 (10): 2390–400. https://doi.org/10.1002/ ij 1955.
Wu Y, Zhou L, Zhang X, et al. Psychological distress and eustress in cancer and cancer treatment: Advances and perspectives. Sci Adv 2022; 8: eabq7982. https://doi.org/10. 1126/sciadv.abq7982.
Mravec B, Tibensky M, Horvathova L. Stress and cancer. Part I: Mechanisms mediating the eff of stressors on cancer. J Neuroimmunol 2020; 346: 577311. https://doi. org/10.1016/j.jneuroim.2020.577311.
Lempesis IG, Georgakopoulou VE, Papalexis P, et al. Role of stress in the pathogenesis of cancer (Review). Int J Oncol 2023; 63 (5): 124. https://doi.org/10.3892/ij 3.5572.
Liu Y, Tian S, Ning B, et al. Stress and cancer: The mecha- nisms of immune dysregulation and management. Front Im- munol 2022; 13: 1032294. https://doi.org/10.3389/fi mu. 2022.1032294.
Ungvari Z, Fekete M, Buda, A, et al. Depression increases cancer mortality by 23–83%: a meta-analysis of 65 studies across fi e major cancer types. GeroScience 2025. https:// doi.org/10.1007/s11357-025-01676-9.
Yan J, Chen Y, Luo M, et al. Chronic stress in solid tumor development: from mechanisms to interventions. J Biomed Sci 2023; 30 (1): 8. https://doi.org/10.1186/s12929-023- 00903-9.
Chekhun VF, Naleskina LA, Kunska LM, Lukianova NY. The driving force of exogenous and endogenous stress as an important factor of metastatic progression of breast can- cer. The role of gelatinases in implementation of invasive and migration processes. Oncology 2024; 26 (3): 157–164. https://doi.org/10.15407/oncology.2024.03.157. (in Ukrai- nian)
Chekhun V, Burda T, Mushii O, et al. Stress-induced modu- lation of the tumor microenvironment: mechanisms and implications for cancer progression. Exp Oncol 2025; 47 (2): 127–142. https://doi.org/10.15407/exp-oncology.2025. 02.127.
Zadvornyi TV, Burda TS, Mushii OM, et al. The role of stress factors in modulating the expression and functional acti- vity of matrix metalloproteinases. Oncology 2025; 27 (2): 111–118. https://doi.org/10.15407/oncology.2025.02.111. (in Ukrainian)
Chekhun VF, Lukianova NY, Kunska LM, et al. Integrated manifestations of cellular stress as a trigger of tumor pro- gression. Cytol Genet 2025; 59: 388–396. https://doi.org/ 10.3103/S0095452725040048.
Predko VV, Somova OO. The influence of the war on the stress level and the strategies for preserving the hardiness of ukrainians. Vcheni zapysky TNU imeni VI Vernadsʹkoho. Seriya: Psykholohiya 2022; 33 (4): 89–98. https://doi.org/ 10.32782/2709-3093/2022.4/16. (in Ukrainian)
Jawad M, Millett C, Sullivan R, et al. The impact of armed conflict on cancer among civilian populations in low- and middle-income countries: A systematic review. Ecancer- medicalscience 2020; 14: 1039. https://doi.org/10.3332/ ecancer.2020.1039.
Korda-Vidić V, Vasilj I, Babić D. The stress of war and breast cancer incidence. Psychiatr Danub 2015; 27 (2): 571–7.
Bøg M, Filges T, Jørgensen AMK. Deployment of person- nel to military operations: impact on mental health and social functioning. Campbell Syst Rev 2018; 14 (1): 1–127. https://doi.org/10.4073/csr.2018.6.
Roberts AL, Huang T, Koenen KC, et al. Posttraumatic stress disorder is associated with increased risk of ovarian cancer: A prospective and retrospective longitudinal cohort study. Cancer Res 2019; 79 (19): 5113–20. https://doi.org/10. 1158/0008-5472.CAN-19-1222.
Yang J, Jiang W. A meta-analysis of the association between post-traumatic stress disorder and cancer risk. Front Psy- chiatry 2023; 14: 1281606. https://doi.org/10.3389/fpsyt. 2023.1281606.
Naugolnyk LB. Psychology of stress: a textbook. Lʹviv: Lʹvivsʹkyy derzhavnyy universytet vnutrishnikh sprav, 2015. 324 р. (in Ukrainian)
Kanczkowski W, Sue M, Wlodarczyk A, Chrousos GP. Hy- pothetical involvement of stress hormones-induced repro-graming of adult stem/progenitor cells in tumorigenesis. Explor Endocr Metab Dis 2024; 1: 122–57. https://doi. org/10.37349/eemd.2024.00012.
Falcinelli M, Thaker PH, Lutgendorf SK, et al. The role of psy- chologic stress in cancer initiation: Clinical relevance and po- tential molecular mechanisms. Cancer Res 2021; 81 (20): 5131– 40. https://doi.org/10.1158/0008-5472.Can-21-0684.
Acevedo-Rodriguez A, Kauffman AS, Cherrington BD, et al. Emerging insights into hypothalamic-pituitary-gonadal axis regulation and interaction with stress signalling. J Neuroen- docrinol 2018; 30 (10): e12590. https://doi.org/10.1111/ jne.12590.
Eckerling A, Ricon-Becker I, Sorski L, et al. Stress and cancer: Mechanisms, significance and future directions. Nat Rev Cancer 2021; 21: 767–85. https://doi.org/10.1038/ s41568-021-00395-5.
Russell G, Lightman S. The human stress response. Nat Rev Endocrinol 2019; 15 (9): 525–34. https://doi.org/10.1038/ s41574-019-0228-0.
Tausk F. Psychoneuro-oncology: How chronic stress grows cancer. Clin Dermatol 2023; 41 (1): 95–104. https://doi. org/10.1016/j.clindermatol.2023.03.008.
Juszczyk G, Mikulska J, Kasperek K, et al. Chronic stress and oxidative stress as common factors of the pathogenesis of depression and alzheimer's disease: The role of antioxidants in prevention and treatment. Antioxidants (Basel) 2021; 10 (9): 1439. https://doi.org/10.3390/antiox10091439.
Reddy VP. Oxidative stress in health and disease. Biomedi- cines 2023; 11 (11): 2925. https://doi.org/10.3390/biomedi- cines11112925.
Spiers JG, Tan LS, Anderson ST, et al. Hepatic homeostasis of metal ions following acute repeated stress exposure in rats. Antioxidants (Basel, Switzerland) 2021; 11 (1): 85. https://doi.org/10.3390/antiox11010085.
Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci 2014; 19 (2): 164–74. 25
Bastian TW, Rao R, Tran PV, Georgieff MK. The eff
of early-life iron deficiency on brain energy metabolism. Neurosci Insights 2020; 15: 2633105520935104. https://
doi.org/10.1177/2633105520935104.
Reid BM, Georgieff MK. The interaction between psycho- logical stress and iron status on early-life neurodevelop- mental outcomes. Nutrients 2023; 15 (17): 3798. https:// doi.org/10.3390/nu15173798.
Wang L, Wang H, Li L, et al. Corticosterone induces dys- regulation of iron metabolism in hippocampal neurons in vitro. Biol Trace Elem Res 2010; 137 (1): 88–95. https:// doi.org/10.1007/s12011-009-8565-9.
Ingale S, Rathored J, Shende S, Wankhade S. The role of calcium homeostasis in modulating the immune response in cancer and infectious diseases. Multidisciplinary Re- views 2024; 8 (2): 2025034. https://doi.org/10.31893/mul- tirev.2025034.
Amantini C, Morelli MB. Editorial: Calcium signaling in can- cer immunity. Front Immunol 2023; 14: 1315490. https:// doi.org/10.3389/fi 3.1315490.
Diercks BP. The importance of Ca2+ microdomains for the adaptive immune response. Biochim Biophys Acta Mol Cell Res 2024; 1871 (5): 119710. https://doi.org/10.1016/j. bbamcr.2024.119710.
Szopa A, Herbet M, Poleszak E, et al. Evaluation of antide- pressive-like behaviours and oxidative stress parameters in mice receiving imipramine-zinc complex compound. Int J Mol Sci 2023; 24 (18): 14157. https://doi.org/10.3390/ ijms241814157.
Jafari F, Mohammadi H, Amani R. The effect of zinc supple- mentation on brain derived neurotrophic factor: A meta-analysis. J Trace Elem Med Biol 2021; 66: 126753. https:// doi.org/10.1016/j.jtemb.2021.126753.
Yosaee S, Soltani S, Esteghamati A, et al. Eff of zinc, vitamin D, and their co-supplementation on mood, serum cortisol, and brain-derived neurotrophic factor in patients with obesity and mild to moderate depressive symptoms: A phase II, 12-wk, 2 × 2 factorial design, double-blind, randomized, placebo-controlled trial. Nutrition 2020; 71: 110601. https://doi.org/10.1016/j.nut.2019.110601.
Michalczyk K, Cymbaluk-Płoska A. The role of zinc and copper in gynecological malignancies. Nutrients 2020; 12 (12): 3732. https://doi.org/10.3390/nu12123732.
Szwiec M, Marciniak W, Derkacz R, et al. Serum levels of copper and zinc and survival in breast cancer patients. Nutrients 2024; 16 (7): 1000. https://doi.org/10.3390/ nu16071000.
Escudero-Cernuda S, Clases D, Eiro N, et al. Quantitative distribution of essential elements and non-essential metals in breast cancer tissues by LA-ICP-TOF-MS. Analytical and bioanalytical chemistry 2025; 417 (2): 361–71. https:// doi.org/10.1007/s00216-024-05652-8.
Saleh SAK, Adly HM, Abdelkhaliq AA, Nassir AM. Serum levels of selenium, zinc, copper, manganese, and iron in prostate cancer patients. Current urology 2020; 14 (1): 44–9. https://doi.org/10.1159/000499261.
Lossow K, Schwarz M, Kipp AP. Are trace element concent- rations suitable biomarkers for the diagnosis of cancer? Redox biology 2021; 42: 101900. https://doi.org/10.1016/j. redox.2021.101900.
Skrajnowska D, Bobrowska-Korczak B. Role of zinc in im- mune system and anti-cancer defense mechanisms. Nutri- ents 2019; 11 (10): 2273. https://doi.org/10.3390/nu1110 2273.
Mandarano AH, McGargill MA. The critical role of copper homeostasis during the immune response. J Immunol 2023; 210 (1): 148.13. https://doi.org/10.4049/jimmunol.210. supp.148.13.
Dhabhar FS. The short-term stress response — Mother na- ture's mechanism for enhancing protection and performance under conditions of threat, challenge, and opportunity. Front Neuroendocrinol 2018; 49: 175–92. https://doi.org/ 10.1016/j.yfrne.2018.03.004.
Alotiby A. Immunology of stress: A review article. J Clin Med 2024; 13 (21): 6394. https://doi.org/10.3390/jcm1321 6394.
Dohi A, Noguchi T, Yamashita M, et al. Acute stress tran- siently activates macrophages and chemokines in cervical lymph nodes. Immunol Res 2024; 72 (2): 212–24. https:// doi.org/10.1007/s12026-023-09409-w.
Vignjević Petrinović S, Milošević MS, Marković D, Mo- mčilović S. Interplay between stress and cancer — A focus on inflammation. Front Physiol 2023; 14: 1119095. https:// doi.org/10.3389/fphys.2023.1119095.
Dantzer R. Neuroimmune interactions: from the brain to the immune system and vice versa. Physiol Rev 2018; 98 (1): 477–504. https://doi.org/10.1152/physrev.00039.2016.
Wu K, Liu Z, Liang J, et al. Discovery of a glucocorticoid receptor (GR) activity signature correlates with immune cell infiltration in adrenocortical carcinoma. J Immunother Cancer 2023; 11 (10): e007528. https://doi.org/10.1136/ jitc-2023-007528.
Shimba A, Ikuta K. Control of immunity by glucocorticoids in health and disease. Semin Immunopathol 2020; 42 (6): 669–80. https://doi.org/10.1007/s00281-020-00827-8.
Taves MD, Ashwell JD. Glucocorticoids in T cell develop- ment, differentiation and function. Nat Rev Immunol 2021; 21 (4): 233–43. https://doi.org/10.1038/s41577-020- 00464-0.
Chhatar S, Lal G. Role of adrenergic receptor signalling in neuroimmune communication. Curr Res Immunol 2021; 2: 202–17. https://doi.org/10.1016/j.crimmu.2021.11.001.
Lorton D, Bellinger DL. Molecular mechanisms underlying β-adrenergic receptor-mediated cross-talk between sympa- thetic neurons and immune cells. Int J Mol Sci 2015; 16 (3): 5635–65. https://doi.org/10.3390/ij 6035635.
Albitre A, Reglero C, González-Muñoz T, Penela P. The stress connection in cancer: the adrenergic fuelling of breast tumors. Current Opinion Physiology 2023; 36: 100720. https://doi.org/10.1016/j.cophys.2023.100720.
Lei Y, Liao F, Tian Y, et al. Investigating the crosstalk be- tween chronic stress and immune cells: implications for enhanced cancer therapy. Front Neurosci 2023; 17: 1321176. https://doi.org/10.3389/fnins.2023.1321176.
Sanders VM. The beta2-adrenergic receptor on T and B lymphocytes: do we understand it yet? Brain Behav Im- mun 2012; 26 (2): 195–200. https://doi.org/10.1016/j.bbi. 2011.08.001.
Somvanshi PR, Mellon SH, Yehuda R, et al. Role of en- hanced glucocorticoid receptor sensitivity in infl tion in PTSD: insights from computational model for circadian- neuroendocrine-immune interactions. Am J Physiol Endo- crinol Metab 2020; 319 (1): E48–E66. https://doi.org/10. 1152/ajpendo.00398.2019.
Khedri M, Samei A, Fasihi-Ramandi M, Taheri RA. The im- munopathobiology of T cells in stress condition: a review. Cell Stress Chaperones 2020; 25 (5): 743–52. https://doi. org/10.1007/s12192-020-01105-0.
Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer 2019; 125 (9): 1417–31.
Bader JE, Voss K, Rathmell JC. Targeting metabolism to improve the tumor microenvironment for cancer immu- notherapy. Mol Cell 2020; 78 (6): 1019–33.
Zhao Y, Jia Y, Shi T, et al. Depression promotes hepatocel- lular carcinoma progression through a glucocorticoid-me- diated upregulation of PD-1 expression in tumor-infiltrating NK cells. Carcinogenesis 2019; 40 (9): 1132–41. https:// doi.org/10.1093/carcin/bgz017.
Chen L, Jondal M, Yakimchuk K. Regulatory effects of dexamethasone on NK and T cell immunity. Infl op- harmacol 2018; 26 (5): 1331–8. https://doi.org/10.1007/ s10787-017-0418-0.
Capellino S, Claus M, Watzl C. Regulation of natural killer cell activity by glucocorticoids, serotonin, dopamine, and epinephrine. Cell Mol Immunol 2020; 17 (7): 705–11. https://doi.org/10.1038/s41423-020-0477-9.
Rocamora-Reverte L, Villunger A, Wiegers GJ. Cell-specific immune regulation by glucocorticoids in murine models of infection and infl tion. Cells 2022; 11 (14): 2126. https://doi.org/10.3390/cells11142126.
Dai S, Mo Y, Wang Y, et al. Chronic stress promotes cancer development. Front Oncol 2020; 10: 1492. https://doi.org/ 10.3389/fonc.2020.01492.
Capelle CM, Chen A, Zeng N, et al. Stress hormone signal- ling inhibits Th1 polarization in a CD4 T-cell-intrinsic manner via mTORC1 and the circadian gene PER1. Im- munology 2022; 165 (4): 428–44. https://doi.org/10.1111/ imm.13448.
Marik PE, Flemmer M. The immune response to surgery and trauma: Implications for treatment. J Trauma Acute Care Surg 2012; 73 (4): 801–8. https://doi.org/10.1097/ TA.0b013e318265cf87.
Kumar P, Bhattacharya P, Prabhakar BS. A comprehensive review on the role of co-signaling receptors and Treg ho- meostasis in autoimmunity and tumor immunity. J Autoim- mun 2018; 95: 77–99.
Bucsek MJ, Hylander BL, Barbi JJ, Repasky EA. Chronic adrenergic stress contributes to metabolic dysfunction and an exhausted phenotype in T cells in the tumor microenvi- ronment. Cancer Immunol Res 2021; 9 (6): 651–64. https:// doi.org/10.1158/2326-6066.CIR-20-0445.
Qiao G, Chen M, Mohammadpour H, et al. Chronic adrener- gic stress contributes to metabolic dysfunction and an ex- hausted phenotype in T cells in the tumor microenviron- ment. Cancer Immunol Res 2021; 9 (6): 651–64.
Acharya N, Madi A, Zhang H, et al. Endogenous gluco- corticoid signaling regulates CD8+ T cell differentiation and development of dysfunction in the tumor microenvi- ronment. Immunity 2020; 53 (3): 658–71.e6. https://doi. org/10.1016/j.immuni.2020.08.005.
Pilipović I, Vujnović I, Stojić-Vukanić Z, et al. Noradrenaline modulates CD4+ T cell priming in rat experimental autoim- mune encephalomyelitis: a role for the α1-adrenoceptor. Immunol Res 2019; 67 (2–3): 223–40. https://doi.org/10. 1007/s12026-019-09082-y.
Mantovani A, Allavena P, Marchesi F, Garlanda C. Mac- rophages as tools and targets in cancer therapy. Nat Rev Drug Discov 2022; 21 (11): 799–820. https://doi.org/10. 1038/s41573-022-00520-5.
Cassetta L, Pollard JW. A timeline of tumour-associated macrophage biology. Nat Rev Cancer 2023; 23 (4): 238–57. https://doi.org/10.1038/s41568-022-00547-1.
Wu Y, Luo X, Zhou Q, et al. The disbalance of LRP1 and SIRPα by psychological stress dampens the clearance of tumor cells by macrophages. Acta Pharm Sin B 2022; 12 (1): 197–209. https://doi.org/10.1016/j.apsb.2021.06.002.
Cheng Y, Tang XY, Li YX, et al. Depression-induced neu- ropeptide Y secretion promotes prostate cancer growth by recruiting myeloid cells. Clin Cancer Res 2019; 25 (8): 2621–32. https://doi.org/10.1158/1078-0432.CCR-18- 2912.
Yuki K. The immunomodulatory mechanism of dexmedeto- midine. Int Immunopharmacol 2021; 97: 107709. https:// doi.org/10.1016/j.intimp.2021.107709.
Sun JX, Xu XH, Jin L. Effects of metabolism on macrophage polarization under different disease backgrounds. Front Im- munol 2022; 13: 880286. https://doi.org/10.3389/fi 2022.880286.
Guo Q, Jin Y, Chen X, et al. NF-κB in biology and targeted therapy: new insights and translational implications. Signal Transduct Target Ther 2024; 9 (1): 53. https://doi.org/ 10.1038/s41392-024-01757-9.
Е. Qin JF, Jin FJ, Li N, et al. Adrenergic receptor β2 activa- tion by stress promotes breast cancer progression through macrophages M2 polarization in tumor microenvironment. BMB Rep 2015; 48 (5): 295–300. https://doi.org/10.5483/ bmbrep.2015.48.5.008.
Park HJ, Lee SC, Park SH. Norepinephrine stimulates M2 macrophage polarization via β2-adrenergic receptor- mediated IL-6 production in breast cancer cells. Biochem Biophys Res Commun 2024; 741: 151087. https://doi.org/ 10.1016/j.bbrc.2024.151087.
Ağaç D, Estrada LD, Maples R, Hooper LV, Farrar JD. The β2-adrenergic receptor controls infl tion by driv- ing rapid IL-10 secretion. Brain Behav Immun 2018; 74: 176–85. https://doi.org/10.1016/j.bbi.2018.09.004.
Sommershof A, Scheuermann L, Koerner J, Groettrup M. Chronic stress suppresses anti-tumor T(CD8+) responses and tumor regression following cancer immunotherapy in a mouse model of melanoma. Brain Behav Immun 2017; 65: 140–9. https://doi.org/10.1016/j.bbi.2017.04.021.
Hunzeker JT, Elftman MD, Mellinger JC, et al. A marked reduction in priming of cytotoxic CD8+ T cells mediated by stress-induced glucocorticoids involves multiple defi ien- cies in cross-presentation by dendritic cells. J Immunol 2011; 186 (1): 183–94. https://doi.org/10.4049/jimmu- nol.1001737.
Pawelec G, Picard E, Bueno V, et al. MDSCs, ageing and infl ing. Cell Immunol 2021; 362: 104297. https:// doi.org/10.1016/j.cellimm.2021.104297.
Mohammadpour H, MacDonald CR, McCarthy PL, et al. β2-adrenergic receptor signaling regulates metabolic path- ways critical to myeloid-derived suppressor cell function within the TME. Cell Rep 2021; 37 (4): 109883. https:// doi.org/10.1016/j.celrep.2021.109883.
An J, Feng L, Ren J, et al. Chronic stress promotes breast carcinoma metastasis by accumulating myeloid-derived suppressor cells through activating β-adrenergic signaling. Oncoimmunol 2021; 10 (1): 2004659. https://doi.org/10. 1080/2162402X.2021.2004659.
Lu Y, Liu H, Bi Y, et al. Glucocorticoid receptor promotes the function of myeloid-derived suppressor cells by suppressing HIF1α-dependent glycolysis. Cell Mol Immunol 2018; 15 (6): 618–29. doi: 10.1038/cmi.2017.5.
Li X, Chen J, Chen YJ, et al. Dexamethasone and lactofer- rin induced PMN-MDSCs relieved inflammatory adverse events of anti-cancer therapy without tumor promotion. Commun Biol 2021; 4: 252. https://doi.org/10.1038/s42003- 021-01769-z.
Zhao Y, Shen X-F, Cao K, et al. Dexamethasone-induced myeloid-derived suppressor cells prolong allo cardiac graft survival through iNOS- and glucocorticoid receptor-depen- dent mechanism. Front Immunol 2018; 9: 282. https://doi. org/10.3389/fi 18.00282.
Zhang Y, Lv N, Li M, et al. Cancer-associated fibroblasts: tumor defenders in radiation therapy. Cell Death Dis 2023; 14 (8): 541. https://doi.org/10.1038/s41419-023-06060-z.
Jia H, Chen X, Zhang L, et al. Cancer associated fibroblasts in cancer development and therapy. J Hematol Oncol 2025; 18: 36. https://doi.org/10.1186/s13045-025-01688-0.
Shan T, Cui X, Li W, et al. Novel regulatory program for norepinephrine-induced epithelial-mesenchymal transition in gastric adenocarcinoma cell lines. Cancer Sci 2014; 105 (7): 847–56. https://doi.org/10.1111/cas.12438.
Nagaraja AS, Dood RL, Armaiz-Pena G, et al. Adrenergic- mediated increases in INHBA drive CAF phenotype and collagens. JCI Insight 2017; 2 (16): e93076. https://doi. org/10.1172/jci.insight.93076.