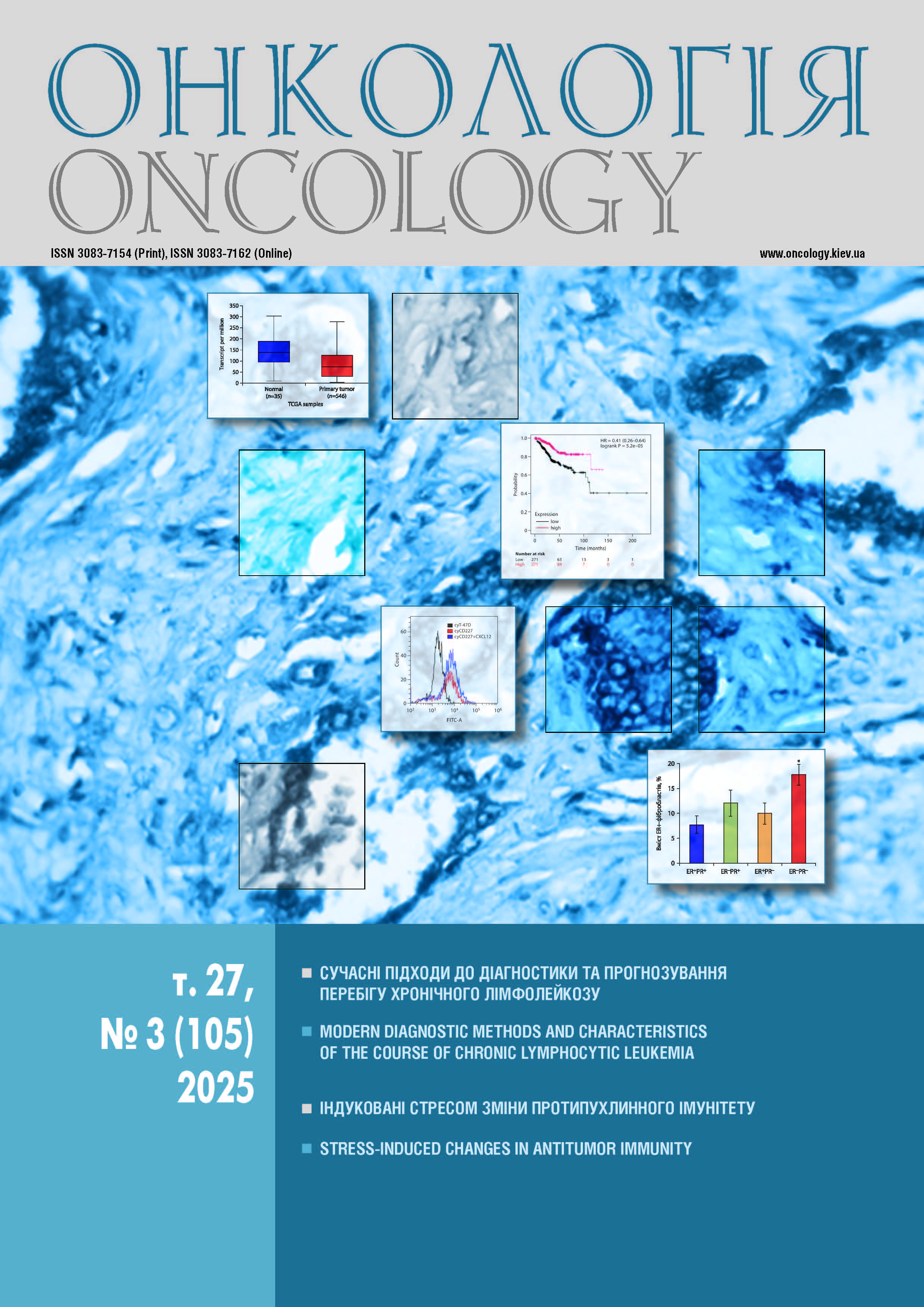
CXCL12 РЕГУЛЮЄ ЕКСПРЕСІЮ CD54, CD326 ТА CD227 В КЛІТИНАХ ЛІНІЙ РАКУ МОЛОЧНОЇ ЗАЛОЗИ
DOI:
https://doi.org/10.15407/oncology.2025.03.190Ключові слова:
рак молочної залози, клітинні лінії, адгезія, CXCL12, СD326 (EpCAM), CD227 (Muc-1), CD54 (ICAM-1)Анотація
Мета: з’ясувати можливість CXCL12 регулювати експресію CD326, CD227 та CD54 в клітинах ліній раку молочної залози. Об’єкт і методи: дослідження проведено на клітинних лініях раку молочної залози T-47D, MCF-7 — люмінального та MDA-MB-231 — тричі негативного молекулярних підтипів. Профіль експресії CD54, CD326 та CD227 вивчали методом проточної цитометрії. Результати: встановлено, що CD326 та CD227 є фенотиповою ознакою клітин ліній люмінального, а CD54 — тричі негативного молекулярних підтипів. За дії CXCL12 відбувається зміна профілю експресії CD54, CD326 та CD227: в клітинах ліній лю- мінального молекулярного підтипу T-47D, MCF-7 відмічено зростання експресії CD54, CD227 та CD326, тоді як в клітинах тричі негативного молекулярного підтипу MDA-MB-231 — ріст експресії CD54 поряд зі зниження експресії CD326. Висновки: активація CXCL12/CXCR4 сигнального шляху в клітинах ліній раку молочної залози регулює експресію CD54, CD326 та CD227, що призводить до набуття клітинами більш агресивного фенотипу.
Посилання
Bianchi ME, Mezzapelle R. The Chemokine receptor CXCR4 in cell proliferation and tissue regeneration. Front Immunol 2020; 11: 2109. https://doi.org/10.3389/ fi109
Masrour M, Moeinafshar A, Poopak A, et al. The role of CXC chemokines and receptors in breast cancer. Clin Exp Med 2025; 25 (1): 128. https://doi.org/10.1007/s10238-025- 01662-7.
Zielińska KA, Katanaev VL. The signaling duo CXCL12 and CXCR4: chemokine fuel for breast cancer tumorigene- sis. Cancers (Basel) 2020; 12 (10): 3071. https://doi.org/ 10.3390/cancers12103071.
Masahiro K, Kitayama J, Kazama S, Nagawa H. Expression pattern of CXC chemokine receptor-4 is correlated with lymph node metastasis in human invasive ductal carcinoma. Breast Cancer Research 2003; 5 (5): R144–50. https://doi.org/10.1186/bcr627.
Yang Y, Li J, Lei W, et al. CXCL12-CXCR4/CXCR7 Axis in Cancer: from Mechanisms to Clinical Applications. Int J Biol Sci 2023; 19 (11): 3341–59. https://doi.org/10.7150/ijs.82317.
Osta W, Chen Y, Mikhitarian K, et al. EpCAM is over-expressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Research 2004; 64 (16): 5818– 24. https://doi.org/10.1158/0008-5472.CAN-04-0754.
Spizzo G, Went P, Dirnhofer S, еt al. High Ep-CAM expres- sion is associated with poor prognosis in node-positive breast cancer. Breast Cancer Res Treat 2004; 86 (3): 207–13. https://doi.org/10.1023/B:BREA.0000036787.59816.01.
Menz A, Lony N, Lennartz M, et al. Epithelial cell adhesion molecule (EpCAM) expression in human tumors: a comparison with pan-cytokeratin and TROP2 in 14,832 tumors. Diagnostics (Basel) 2024; 14 (10): 1044. https://doi.org/10.3390/diagnostics14101044.
Mukherjee S, Richardson A, Rodriguez-Canales J, et al. Identification of EpCAM as a molecular target of prostate cancer stroma. Am J Pathol 2009; 175 (6): 2277–87. https://doi.org/10.2353/ajpath.2009.090013.
Fong D, Moser P, Kasal A, et al. Loss of membranous expression of the intracellular domain of EpCAM is a frequent event and predicts poor survival in patients with pancrea- tic cancer. Histopathol 2014; 64 (5): 683–92. https://doi.org/10.1111/his.12307.
Spizzo G, Went P, Dirnhofer S, et al. Overexpression of epithelial cell adhesion molecule (Ep-CAM) is an independent prognostic marker for reduced survival of patients with epithelial ovarian cancer. Gynecol Oncol 2006; 103 (2): 483–8. https://doi.org/10.1016/j.ygyno.2006.03.035.
Went P, Vasei M, Bubendorf L, et al. Frequent high-level expression of the immunotherapeutic target Ep-CAM in colon, stomach, prostate and lung cancers. British J Can- cer 2006; 94 (1): 128–35. https://doi.org/10.1038/sj.bjc.6602924.
Went P, Dirnhofer S, Salvisberg T, et al. Expression of epithelial cell adhesion molecule (EpCam) in renal epithelial tumors. Am J Surg Pathol 2005; 29 (1): 83–8. https://doi.org/10.1097/01.pas.0000.146028.70868.7a.
Wen K, Sun P, Chou H, et al. The role of EpCAM in tumor progression and the clinical prognosis of endometrial carcinoma. Gynecol Oncol 2018; 148 (2): 383–92. https:// doi.org/10.1016/j.ygyno.2017.11.033.
Wu Q, Wang J, Liu Y, et al. Epithelial cell adhesion molecule and epithelial-mesenchymal transition are associated with vasculogenic mimicry, poor prognosis, and metastasis of triple negative breast cancer. Int J Clin Exp Pathol 2019; 12 (5): 1678–89.
Lan Y, Ni W, Tai G. Expression of MUC1 in diff rent tumours and its clinical significance (Review). Mol Clin Oncol 2022; 17 (6): 161. https://doi.org/10.3892/mco.2022.2594.
Rahn J, Dabbagh L, Pasdar M, Hugh J. The importanceof MUC1 cellular localization in patients with breast carcinoma: an immunohistologic study of 71 patients and review of the literature. Cancer 2001; 91 (11): 1973–82. https://doi.org/10.1002/1097-0142(20010601)91:11<1973::aid-cncr 1222>3.0.co;2-a.
Kufe D. MUC1-C oncoprotein as a target in breast cancer: activation of signaling pathways and therapeutic approaches. Oncogene 2013; 32 (9): 1073–81. https://doi.org/10.1038/ onc.2012.158.
Reina M, Espel E. Role of LFA-1 and CD54 in cancer. Cancers (Basel) 2017; 9 (11): 153. https://doi.org/10.3390/ cancers9110153.
Benedicto A, Romayor, Arteta B. Role of liver CD54 in metastasis. Oncol Let 2017; 14 (4): 3883–92. https://doi.org/10.3892/ol.2017.6700.
Tachimori A, Yamada N, Sakate G, et al. Up regulation of CD54gene expression inhibits tumour growth and liver metastasis in colorectal carcinoma. Eur J Cancer 2005; 41 (12): 1802–10. https://doi.org/10.1016/j.ejca.2005.04.036.
Ramer R, Bublitz K, Freimuth F, et al. Cannabidiol inhibits lung cancer cell invasion and metastasis via intercellular adhesion molecule-1. FASEB J 2012; 26 (4): 1535–48. https://doi.org/10.1096/fj.11-198184.
Kang Н, Watkins G, Parr C, et al. Stromal cell derived fac- tor-1: its influence on invasiveness and migration of breast cancer cells in vitro, and its association with prognosis and survival in human breast cancer. Breast Cancer Res 2005; 7 (4): R402–10. https://doi.org/10.1186/bcr1022.
Gordiienko I, Lykhova O, Shcherbina V, Shlapatska L. SLAMF1/CD150 expression and topology in prostate and breast cancer cell lines. Exp Oncol 2021; 43 (4): 312–16. https://doi.org/10.32471/exp-oncology.2312-8852.vol-43- no-4.17010.
Kuhn S, Koch M, Nubel T, et al. A complex of EpCAM, claudin-7, CD44 variant isoforms, and tetraspanins promotes colorectal cancer progression. Mol Cancer Res 2007; 5 (6): 553–67. https://doi.org/10.1158/1541-7786.MCR-06-0384.
Pop M, Bartoș D, Fiț A, et al. Detection of epithelial specific cell adhesion molecules in colon cancer and the correlation with clinical and pathological characteristics EpCAM expression in colon cancer. Ann Ital Chir 2019; 90: 318–23.
Schmidt M. Prognostic eff of epithelial cell adhesion molecule overexpression in untreated node-negative breast cancer. Clin Cancer Res 2008; 14 (18): 5849–55. https:// doi.org/10.1158/1078-0432.CCR-08-0669.
Gires O, Pan M, Schinke H, et al. Expression and function of epithelial cell adhesion molecule EpCAM: where are we after 40 years? Cancer Metastasis Rev 2020; 39 (3): 969–87. https://doi.org/10.1007/s10555-020-09898-3.
Gun B, Melchers L, Ruiters M, et al. EpCAM in carcinogenesis: the good, the bad or the ugly. Carcinogenesis 2010; 31 (11): 1913–21. https://doi.org/10.1093/carcin/bgq187.
Martowicz A, Spizzo G, Gastl G, Untergasser G. Рheno- type-dependent effects of EpCAM expression on growth and invasion of human breast cancer cell lines. BMC Cancer 2012; 12: 501. https://doi.org/10.1186/1471-2407- 12-501.
Bui T, Wiesolek H, Sumagin R. ICAM-1: A master regulator of cellular responses in infl tion, injury resolution, and tumorigenesis. J Leukoc Biol 2020; 108 (3): 787–99. https://doi.org/10.1002/JLB.2MR0220-549R.
Yuan X, Wu H, Li X, et al. SDF-1α/CXCR4 signaling promotes capillary tube formation of human retinal vascular endothelial cells by activating ERK1/2 and PI3K pathways in vitro. Mol Med Rep 2022; 26 (4): 305. https://doi.org/10.3892/mmr.2022.12821.
Leccia F, Nardone A, Corvigno S, et al. Cytometric and biochemical characterization of human breast cancer cells reveals heterogeneous myoepithelial phenotypes. Cytometry A 2012; 81 (11): 960–2. https://doi.org/10.1002/cyto.a.2209.
Huang Z, Yu P, Tang J. Characterization of triple-negative breast cancer MDA-MB-231 cell spheroid model. Onco Targets Ther 2020; 13: 5395–405. https://doi.org/10.2147/ OTT.S249756.
Zhang Y, Fan J, Wang X, et al. Role of CD54 in triple-negative breast cancer. Open Med (Wars) 2024; 19 (1): 20240969. https://doi.org/10.1515/med-2024-0969.
Wei H, Wang Z, Kuang Y, et al. Intercellular adhesion molecule-1 as target for CAR-T-cell therapy of triple-negative breast cancer. Front Immunol 2020; 11: 573823. https://doi.org/10.3389/fi73823.
Iqbal M, Otsuyama K, Shamsasenjan K, et al. Constitutively lower expressions of CD54 on primary myeloma cells and their different localizations in bone marrow. Eur J Haematol 2009; 83 (4): 302–12. https://doi.org/10.1111/j.1600-0609. 2009.01284.x.
Xing B, Yang L, Cui Y. Lidocaine inhibited migration of NSCLCA549 cells via the CXCR4 regulation. Cancer Bio-mark 2022; 33 (3): 317–30. https://doi.org/10.3233/CBM- 210249.
Tung S, Chang S, Chou M, Huang W, et al. CXC chemokine ligand 12/stromal cell-derived factor-1 regulates cell adhesion in human colon cancer cells by induction of intercellular adhesion molecule-1. J Biomed Sci 2012; 19 (1): 91. https://doi.org/10.1186/1423-0127-19-91.
Ryuko K, Schol D, Snijdewint F, et al. Characterization of a new MUC1 monoclonal antibody (VU-2-G7) directed to the glycosylated PDTR sequence of MUC1.Tumour Biol 2000; 21 (4): 197–210. https://doi.org/10.1159/000030126.
Engelstaedter V, Heublein S, Schumacher A, et al. Mucin-1 and its relation to grade, stage and survival in ovarian carcinoma patients. BMC Cancer 2012; 12: 600. https://doi.org/10.1186/1471-2407-12-600.
Iizuka M. Altered intracellular region of MUC1 and disrupted correlation of polarity-related molecules in breast cancer subtypes. Cancer Sci 2015; 106 (3): 307–14. https:// doi.org/10.1111/cas.12596.
Choi I, Ahn do W, Choi J, et al. Regulation of airway inflammation by G-protein regulatory motif peptides of AGS3 protein. Sci Rep 2016; 6: 27054. https://doi.org/10.1038/ srep27054.
Semba R, Horimoto Y, Sakata-Matsuzawa M, et al. Possible correlation of apical localization of MUC1 glycoprotein with luminal A-like status of breast cancer. Sci Rep 2023; 13 (1): 5281. https://doi.org/10.1038/s41598-023-32579-4.