Перемога мРНК-вакцин над пандемією коронавірусу SARS-CoV-2, який викликає захворювання COVID-19, або як синтетична мРНК прослизнула повз вроджений імунний захист клітини
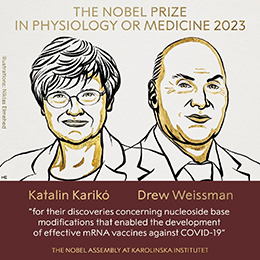
Нобелівська премія з фізіології або медицини 2023 року
DOI:
https://doi.org/10.15407/visn2023.12.003Ключові слова:
Нобелівська премія з фізіології або медицини 2023 року, Каталін Каріко, Дрю Вайсман, пандемія SARS-CoV-2, COVID-19, мРНК-вакцинаАнотація
Нобелівську премію з фізіології або медицини у 2023 р. присуджено двом вченим: угорсько-американському біохіміку Каталін Каріко (Katalin Karikó) та американському імунологу Дрю Вайсману (Drew Weissman) з Пенсільванського університету в Філадельфії (Каталін Каріко одночасно працює в Угорщині в Сегедському університеті) «за відкриття щодо модифікацій нуклеозидних основ, які дозволили розробити ефективні мРНК-вакцини проти COVID-19». Як зазначено у пресрелізі Нобелівського комітету, відкриття цьогорічних нобелівських лауреатів мали вирішальне значення для створення ефективних мРНК-вакцин проти COVID-19 під час пандемії, що трапилася на початку 2020 р. Їхні революційні відкриття, які фундаментально змінили наше розуміння того, як мРНК взаємодіє з імунною системою, сприяли тому, що безпрецедентно швидко вдалося розробити вакцини для боротьби з однією з найбільших за останній час загроз здоров'ю людини.
Посилання
Tang D.C., DeVit M., Johnston S.A. Genetic immunization is a simple method for eliciting an immune response. Nature. 1992. 356(6365): 152—154. https://doi.org/10.1038/356152a0
Martinon F., Krishnan S., Lenzen G., Magné R., Gomard E., Guillet J.G., Lévy J.P., Meulien P. Induction of virus-specific cytotoxic T lymphocytes in vivo by liposome-entrapped mRNA. Eur. J. Immunol. 1993. 23(7): 1719—1722. https://doi.org/10.1002/eji.1830230749
Liu M.A., Ulmer J.B. Human clinical trials of plasmid DNA vaccines. Adv. Genet. 2005. 55: 25—40. https://doi.org/10.1016/S0065-2660(05)55002-8
Brenner S., Jacob F., Meselson M. An unstable intermediate carrying information from genes to ribosomes for protein synthesis. Nature. 1961. 190: 576—581. https://doi.org/10.1038/190576a0
Gros F., Hiatt H., Gilbert W., Kurland C.G., Risebrough R.W., Watson J.D. Unstable ribonucleic acid revealed by pulse labelling of Escherichia coli. Nature. 1961. 190: 581—585. https://doi.org/10.1038/190581a0
Lockard R.E., Lingrel J.B. The synthesis of mouse hemoglobin beta-chains in a rabbit reticulocyte cell-free system programmed with mouse reticulocyte 9S RNA. Biochem. Biophys. Res. Commun. 1969. 37(2): 204—212. https://doi.org/10.1016/0006-291x(69)90720-7
Gurdon J.B., Lane C.D., Woodland H.R., Marbaix G. Use of frog eggs and oocytes for the study of messenger RNA and its translation in living cells. Nature. 1971. 233(5316): 177—182. https://doi.org/10.1038/233177a0
Wolff J.A., Malone R.W., Williams P., Chong W., Acsadi G., Jani A., Felgner P.L. Direct gene transfer into mouse muscle in vivo. Science. 1990. 247(4949 Pt. 1): 1465—1468. https://doi.org/10.1126/science.1690918
Krieg P.A., Melton D.A. Functional messenger RNAs are produced by SP6 in vitro transcription of cloned cDNAs. Nucleic Acids Res. 1984. 12(18): 7057—7070. https://doi.org/10.1093/nar/12.18.7057
Dunn J.J., Studier F.W. Complete nucleotide sequence of bacteriophage T7 DNA and the locations of T7 genetic elements. J. Mol. Biol. 1983. 166(4): 477—535. https://doi.org/10.1016/s0022-2836(83)80282-4
Studier F.W., Moffatt B.A. Use of bacteriophage T7 RNA polymerase to direct selective high-level expression of cloned genes. J. Mol. Biol. 1986. 189(1): 113—130. https://doi.org/10.1016/0022-2836(86)90385-2
Langer R., Folkman J. Polymers for the sustained release of proteins and other macromolecules. Nature. 1976. 263(5580): 797—800. https://doi.org/10.1038/263797a0
Ostro M.J., Giacomoni D., Lavelle D., Paxton W., Dray S. Evidence for translation of rabbit globin mRNA after liposome-mediated insertion into a human cell line. Nature. 1978. 274(5674): 921—923. https://doi.org/10.1038/274921a0
Felgner P.L., Gadek T.R., Holm M., Roman R., Chan H.W., Wenz M., Northrop J.P., Ringold G.M., Danielsen M. Lipofection: a highly efficient, lipid-mediated DNA-transfection procedure. Proc. Natl. Acad. Sci. USA. 1987. 84(21): 7413—7417. https://doi.org/10.1073/pnas.84.21.7413
Malone R.W., Felgner P.L., Verma I.M. Cationic liposome-mediated RNA transfection. Proc. Natl. Acad. Sci. USA. 1989. 86(16): 6077—6081. https://doi.org/10.1073/pnas.86.16.6077
Gref R., Minamitake Y., Peracchia M.T., Trubetskoy V., Torchilin V., Langer R. Biodegradable long-circulating polymeric nanospheres. Science. 1994. 263(5153): 1600—1603. https://doi.org/10.1126/science.8128245
Zhou X., Berglund P., Rhodes G., Parker S.E., Jondal M., Liljeström P. Self-replicating Semliki Forest virus RNA as recombinant vaccine. Vaccine. 1994. 12(16): 1510—1514. https://doi.org/10.1016/0264-410x(94)90074-4
Jirikowski G.F., Sanna P.P., Maciejewski-Lenoir D., Bloom F.E. Reversal of diabetes insipidus in Brattleboro rats: intrahypothalamic injection of vasopressin mRNA. Science. 1992. 255(5047): 996—998. https://doi.org/10.1126/science.1546298
Karikó K., Keller J.M., Harris V.A., Langer D.J., Welsh F.A. In vivo protein expression from mRNA delivered into adult rat brain. J. Neurosci. Methods. 2001. 105(1): 77—86. https://doi.org/10.1016/s0165-0270(00)00355-1
Weissman D., Ni H., Scales D., Dude A., Capodici J., McGibney K., Abdool A., Isaacs S.N., Cannon G., Karikó K. HIV gag mRNA transfection of dendritic cells (DC) delivers encoded antigen to MHC class I and II molecules, causes DC maturation, and induces a potent human in vitro primary immune response. J. Immunol. 2000. 165(8): 4710—4717. https://doi.org/10.4049/jimmunol.165.8.4710
Ni H., Capodici J., Cannon G., Communi D., Boeynaems J.M., Karikó K., Weissman D. Extracellular mRNA induces dendritic cell activation by stimulating tumor necrosis factor-alpha secretion and signaling through a nucleotide receptor. J. Biol. Chem. 2002. 277(15): 12689—12696. https://doi.org/10.1074/jbc.M110729200
Akira S., Hemmi H. Recognition of pathogen-associated molecular patterns by TLR family. Immunol. Lett. 2003. 85(2): 85—95. https://doi.org/10.1016/s0165-2478(02)00228-6
Diebold S.S., Kaisho T., Hemmi H., Akira S., Reis e Sousa C. Innate antiviral responses by means of TLR7-mediated recognition of single-stranded RNA. Science. 2004. 303(5663): 1529—1531. https://doi.org/10.1126/science.1093616
Heil F., Hemmi H., Hochrein H., Ampenberger F., Kirschning C., Akira S., Lipford G., Wagner H., Bauer S. Species-specific recognition of single-stranded RNA via toll-like receptor 7 and 8. Science. 2004. 303(5663): 1526—1529. https://doi.org/10.1126/science.1093620
Hemmi H., Takeuchi O., Kawai T., Kaisho T., Sato S., Sanjo H., Matsumoto M., Hoshino K., Wagner H., Takeda K., Akira S. A Toll-like receptor recognizes bacterial DNA. Nature. 2000. 408(6813): 740—745. https://doi.org/10.1038/35047123
Karikó K., Ni H., Capodici J., Lamphier M., Weissman D. mRNA is an endogenous ligand for Toll-like receptor 3. J. Biol. Chem. 2004. 279(13): 12542—12550. https://doi.org/10.1074/jbc.M310175200
Karikó K., Buckstein M., Ni H., Weissman D. Suppression of RNA recognition by Toll-like receptors: the impact of nucleoside modification and the evolutionary origin of RNA. Immunity. 2005. 23(2): 165—175. https://doi.org/10.1016/j.immuni.2005.06.008
Karikó K., Muramatsu H., Welsh F.A., Ludwig J., Kato H., Akira S., Weissman D. Incorporation of pseudouridine into mRNA yields superior nonimmunogenic vector with increased translational capacity and biological stability. Mol. Ther. 2008. 16(11): 1833—1840. https://doi.org/10.1038/mt.2008.200
Anderson B.R., Muramatsu H., Nallagatla S.R., Bevilacqua P.C., Sansing L.H., Weissman D., Karikó K. Incorporation of pseudouridine into mRNA enhances translation by diminishing PKR activation. Nucleic Acids Res. 2010. 38(17): 5884—5892. https://doi.org/10.1093/nar/gkq347
Anderson B.R., Muramatsu H., Jha B.K., Silverman R.H., Weissman D., Karikó K. Nucleoside modifications in RNA limit activation of 2′-5′-oligoadenylate synthetase and increase resistance to cleavage by RNase L. Nucleic Acids Res. 2011. 39(21): 9329—9338. https://doi.org/10.1093/nar/gkr586
Karikó K., Muramatsu H., Ludwig J., Weissman D. Generating the optimal mRNA for therapy: HPLC purification eliminates immune activation and improves translation of nucleoside-modified, protein-encoding mRNA. Nucleic Acids Res. 2011. 39(21): e142. https://doi.org/10.1093/nar/gkr695
Baiersdörfer M., Boros G., Muramatsu H., Mahiny A., Vlatkovic I., Sahin U., Karikó K. A Facile Method for the Removal of dsRNA Contaminant from In Vitro-Transcribed mRNA. Mol. Ther. Nucleic Acids. 2019. 15: 26—35. https://doi.org/10.1016/j.omtn.2019.02.018
Hoerr I., Obst R., Rammensee H.G., Jung G. In vivo application of RNA leads to induction of specific cytotoxic T lymphocytes and antibodies. Eur. J. Immunol. 2000. 30(1): 1—7. https://doi.org/10.1002/1521-4141(200001)30:1<1::AID-IMMU1>3.0.CO;2-#
Dolgin E. The tangled history of mRNA vaccines. Nature. 2021. 597(7876): 318—324. https://doi.org/10.1038/d41586-021-02483-w
Pardi N., Hogan M.J., Pelc R.S., 33 coauthors, Weissman D. Zika virus protection by a single low-dose nucleoside-modified mRNA vaccination. Nature. 2017. 543(7644): 248—251. https://doi.org/10.1038/nature21428
Bahl K., Senn J.J., Yuzhakov O., Bulychev A., Brito L.A., Hassett K.J., Laska M.E., Smith M., Almarsson Ö., Thompson J., Ribeiro A.M., Watson M., Zaks T., Ciaramella G. Preclinical and clinical demonstration of immunogenicity by mRNA vaccines against H10N8 and H7N9 influenza viruses. Mol. Ther. 2017. 25(6): 1316—1327. https://doi.org/10.1016/j.ymthe.2017.03.035
Komisarenko S.V. Scientists’ pursuit for SARS-COV-2 coronavirus: strategies against pandemic. Ukr. Biochem. J. 2020. 92(6): 5—52. https://doi.org/10.15407/ubj92.06.005
Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.L., Abiona O., Graham B.S., McLellan J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020. 367(6483): 1260—1263. https://doi.org/10.1126/science.abb2507
Krynina O.I., Romaniuk S.I., Gorbatiuk O.B., Korchynskyi O.H., Rebriiev А.V., Kulyk Ya.S., Kozadaieva Ye.O., Siromolot A.A., Guzyk M.M., Kolybo D.V., Komisarenko S.V. Production of recombinant SARS-CoV-2 proteins and diphtheria toxoid CRM197-based fusion. Ukr. Biochem. J. 2021. 93(6): 31—45. https://doi.org/10.15407/ubj93.06.031
Qiao H., Pelletier S.L., Hoffman L., Hacker J., Armstrong R.T., White J.M. Specific single or double proline substitutions in the "spring-loaded" coiled-coil region of the influenza hemagglutinin impair or abolish membrane fusion activity. J. Cell. Biol. 1998. 141(6): 1335—1347. https://doi.org/10.1083/jcb.141.6.1335
Sahin U., Muik A., Derhovanessian E., 38 coauthors, Türeci Ö. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature. 2020. 586(7830): 594—599. https://doi.org/10.1038/s41586-020-2814-7
Corbett K.S., Edwards D.K., Leist S.R., 58 coauthors, Graham B.S. SARS-CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature. 2020. 586(7830): 567—571. https://doi.org/10.1038/s41586-020-2622-0
Polack F.P., Thomas S.J., Kitchin N., 24 coauthors, Gruber W.C., C4591001 Clinical Trial Group. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020. 383(27): 2603—2615. https://doi.org/10.1056/NEJMoa2034577
Husby A., Køber L. COVID-19 mRNA vaccination and myocarditis or pericarditis. Lancet. 2022. 399(10342): 2168—2169. https://doi.org/10.1016/S0140-6736(22)00842-X
Qu L., Yi Z., Shen Y., 28 coauthors, Wei W. Circular RNA vaccines against SARS-CoV-2 and emerging variants. Cell. 2022. 185(10): 1728—1744.e16. https://doi.org/10.1016/j.cell.2022.03.044
O'Connor M.A., Hawman D.W., Meade-White K., 23 coauthors, Erasmus J.H. A replicon RNA vaccine can induce durable protective immunity from SARS-CoV-2 in nonhuman primates after neutralizing antibodies have waned. PLoS Pathog. 2023. 19(4): e1011298. https://doi.org/10.1371/journal.ppat.1011298
Sun B., Wu W., Narasipura E.A., Ma Y., Yu C., Fenton O.S., Song H. Engineering nanoparticle toolkits for mRNA delivery. Adv. Drug Deliv. Rev. 2023. 200: 115042. https://doi.org/10.1016/j.addr.2023.115042
Conde J., Langer R., Rueff J. mRNA therapy at the convergence of genetics and nanomedicine. Nat. Nanotechnol. 2023. 18(6): 537—540. https://doi.org/10.1038/s41565-023-01347-w
Dolgin E., Ledford H. mRNA COVID vaccines saved lives and won a Nobel — what’s next for the technology? https://www.nature.com/articles/d41586-023-03119-x
Arevalo C.P., Bolton M.J., Le Sage V., 13 coauthors, Weissman D., Hensley S.E. A multivalent nucleoside-modified mRNA vaccine against all known influenza virus subtypes. Science. 2022. 378(6622): 899—904. https://doi.org/10.1126/science.abm0271
Cohen J. ‘Landmark’ study finds artificial antibodies can protect against malaria. Science News. https://doi.org/10.1126/science.abl8960
Egan K.P., Awasthi S., Tebaldi G., Hook L.M., Naughton A.M., Fowler B.T., Beattie M., Alameh M.G., Weissman D., Cohen G.H., Friedman H.M. A trivalent HSV-2 gC2, gD2, gE2 nucleoside-modified mRNA-LNP vaccine provides outstanding protection in mice against genital and non-genital HSV-1 infection, comparable to the same antigens derived from HSV-1. Viruses. 2023. 15(7): 1483. https://doi.org/10.3390/v15071483
Sahin U., Oehm P., Derhovanessian E., 37 coauthors, Türeci Ö. An RNA vaccine drives immunity in checkpoint-inhibitor-treated melanoma. Nature. 2020. 585(7823): 107—112. https://doi.org/10.1038/s41586-020-2537-9
Cromer D., Reynaldi A., Steain M., Triccas J.A., Davenport M.P., Khoury D.S. Relating in vitro neutralization level and protection in the CVnCoV (CUREVAC) Trial. Clin. Infect. Dis. 2022. 75(1): e878—e879. https://doi.org/10.1093/cid/ciac075